As I start this story, it is May 14, 2024, six days after my ablation. I never believed this story would have to be written in 4 parts, but so be it, you will have all the information now and I hope it might be useful for your health and state of mind. And, as usual, hopefully a little funny.
I left off in The Heart Stories Part 3 after being discharged from the hospital after experiencing two cardioversions. They did not fix me but gave me hope that the next procedure would work. After all you must always have hope.
An ablation uses heat or cold energy to create tiny scars in the heart. The scars block faulty heart signals and restore a typical heartbeat, thus bringing you into a normal sinus rhythm.
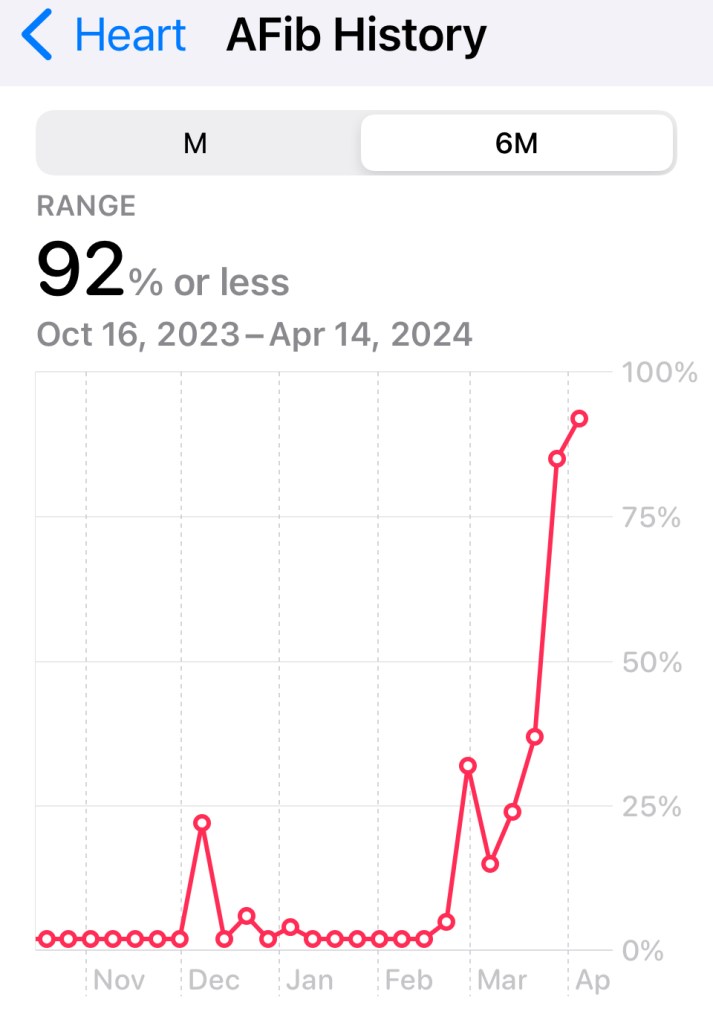
Part 3 detailed the rise in my atrial fibrilation from 2% to 93% after my TAVR procedure. I understood that sometimes that happens. What I didn’t realize is that you cannot function with 93% afib, or at least I could not. After the cardio versions they started me on a medication called amiodarone. It is a powerful drug and my doctor mentioned that googling it might not be a good idea. I was infused with this drug slowly before leaving the hospital over a 24 hour period and now I would be taking two 400 mg per day dose. At this point my ablation was scheduled for May 8th, the day after my 76th birthday–and I was looking forward to it.
As each day passed after the cardio versions, I got weaker, dizzier and basically unable to do anything worthwhile. My heart was in a constant flutter. Depression set in quickly and I withdrew from everything. I think this is important because I think the depression and anxiety was worse than my heart fluttering. I don’t think I ever experienced such a feeling and hope to never again feel that way.
Aside: I usually put my stories through an Artificial Intelligence filter to check any discrepancies and it provides feedback about the story. The AI feedback from Part 3 was the ending should be more positive. I will take that feedback as a gift.
Between April 24 and May 8th was difficult. There were some things that I was determined to do. For one, my friend who passed in January was going to be celebrated at a gathering on a Sunday at the restaurant at the Public Theatre. What was odd was I was also scheduled to go to a show at the same theatre on Tuesday of that week. I fought my anxiety to go to the celebration of my friend’s life, but Mike was driving and I could escape at any time if necessary. The gathering included some of my colleagues and friends who I haven’t seen in years and they were all there for my dear friend singing praises of her life–which was indeed too short and quite unexpected at the time. During this period of time, I would get manic and talk louder than usual and a lot. I already talk a lot, so this was very obvious to me. It was good to be with people I loved that could excuse this behavior.
That was Sunday and now I was deliberating about whether I would go to that theatre again for a show called Generation Women on Tuesday night. I have been to a few other similar shows and it was 6 women covering 6 decades telling a specific story. The story they were asked to provide was the “worst decision they ever made.” A good friend called me and said she would pick me up at my house and drive to Manhattan and then drive me home and then continue on to her house in New Jersey. I thanked her and said I would call her on Monday and let her know. I started to feel anxious about going and called and declined her kind offer. On Tuesday, I decided I needed to push myself, so another call to my friend that I changed my mind. She drove to me, I drove to the city and back to my house. Having a good friend supporting me was a blessing and I will never forget her kindness. I am actually unsure how I did this, but I do know that you can fight anxiety with the help of others. It was a good night with 6 friends having dinner and seeing a great show with stories both happy, sad, funny and serious. I solemnly thought if this was my last night, I would leave this earth a happy camper.
I cannot explain how much love I received from friends during this time. By putting my stories out there, I received prayers, love, support, compassionate from oh so many people. I will be forever grateful for them.
The rest of the week and weekend passed slowly and tediously, but I was definitely ready for this procedure and putting this all behind me. My birthday was here–I didn’t even have a cocktail–for sure I will make up for that. I received the call from the hospital which said show up at 9:30 am on May 8. I knew that meant my procedure would happen a few hours after that. For some strange reason, or from all the prayers and thoughts I was getting, when I got to the hospital I was no longer anxious. I was in their hands and today it would be over.
I was told that the TAVR is so much more intrusive than the ablation. TAVR goes through arteries; ablations goes through veins. OK, no kneeling on my groin to stop the bleeding–that definitely was a plus. It was also under general anesthesia which is not great, but I would rather be asleep than awake.
On arrival, I was greeted by RN Nicole who said she would be my caregiver until I was taken in. Nicole and I realized we lived in the same neighborhood. She had twin boys, about 1 year old and a daughter about 6. We talked about schooling and churches. Staten Island is a small place. She was in the same parish as me [the new parish that I fled to in December]. She asked why I left my original parish since it was closer to my house and I explained that the pastor drove me out by a crazy-ass sermon. She actually grew up on the block where his mom lived and had heard some not-so-kind comments about him recently. This was not surprising to me, but I was not going to sit around badmouthing a priest before this procedure. I do say a Hail Mary for this guy each morning….I pray that he would “be better.” [That will be the last time in my life that I use a phrase from Melania Trump, but it seemed too perfect not to.]
I met Jason and two or three other caregivers–everyone was friendly. My bed was positioned right in front of the door where another person was receiving an ablation. So this patient went in sometime before 9:00 am and it was now 12:30 pm and he was still in there. It is not a sterile room, which surprised me but there was so much equipment and people walked in and our a few times. My sister had an ablation not too long ago and said she was astounded by the amount of people and technical equipment in a small room. The room I could peek into on occasion was also small, with monitors, computers and people. It was also darkened. I always thought of operating rooms being very bright–this was the opposite.
Aside: At a point while I was waiting, a crew of administrators and hospital personnel came into this room to talk about a rebuild that was going to happen. They were in there a long time talking about moving equipment, number of beds, etc. I found it amusing at first, but quickly tired of the noise and people.
Finally, the patient was wheeled out of the room. From my perspective he looked OK and was groggy but awake. There was another patient in this room; a woman who only spoke Russian. I was pleasantly surprised that they had a special TV screen that they rolled around to patients who needed a translator. I could hear the man on the monitor translating everything the doctor was saying to the patient. It was almost like a zoom call. I had never seen that before and really never thought about it. Good to learn new things.
My doctor and the anesthesiologist were the same as the previous patient. He greeted me and apologized for the delay. I urged him to go take a break, have lunch and be fully refreshed for my procedure. I really wasn’t kidding–I was dead serious. I signed papers for the anesthesiologist and would eventually sign some releases from my doctor. He said he would get some lunch and be back as soon as he could. I nonchalantly told him to take his time. At this point I was already there 4 hours and could wait a bit more.
Everyone returned at about 1:30 pm and the lead nurse from the ablation room came to speak with me. Her name was Joy–I instantly liked her. She was professional, kind and compassionate–you really can’t ask for more than that. She explained that they would be putting many patches on me. My first thought was I was still trying to get the sticky tape off me from the cardioversions and now Joy was explaining there would be many many stickies on me. The internet defines these stickies as “The grounding pad–adhered to the patient’s skin away from the surgical site—is intended to safely return the electrical current from the patient back to the generator through a cord or cable.” Simply put, the sticky pads are grounding mechanisms to keep you from being electrocuted during the procedure. OK, now. I already know more than I need to know.
Joy allowed me to walk into the room, it was only about 100 feet from where my bed was. The bed in this room was tiny and looked totally uncomfortable. But alas, there were pillows that inflated around your body and it was not that uncomfortable. I hopped on the table and Joy started explaining each and every ground pad. I wondered how long this would take, because by now I was starving, wanting to be asleep and having this procedure over. Joy introduced me to the team of about 9 people. They included RNs, doctors, tech people plus me. I always like to look mobile when in a hospital. I believe it is important for those treating you to know, you walked, you talked and you wanted to leave in better shape then when you arrived.
Once I laid down, they put a few more electrodes on my legs, feet, arms, just about everywhere there was skin. Then the mask and the direction to breathe deeply.
5 hours later–I felt a tube being pulled from my throat–not painful–just realization that I was awake and the procedure was over. I didn’t know what time it was but it was the first question I asked. It was 7:30 pm. Wow! That took a long time! My doctor told me he called Mike and that everything went fine. I knew from previous conversations, this procedure would not relieve me immediately. The scarring of the heart had to form. I felt I was in sinus rhythm and that was a good thing. I now had to stay on my back for about 4 hours. No problem, I was actually tired and very groggy–general anesthesia does that to you.
In about an hour, they wheeled me into a room on the cardiac unit. For some reason I got a suite with a 20 foot window looking over the Verazzano Bridge and the water. Lovely! There would be no food tonight and I was ok with that. A nutritionist came by and took my breakfast order. I was not interested in being on my phone, or listening to a podcast, or doing anything but sleeping.
I woke up for sunrise which was beautiful. I moved around a bit and felt OK, there was no part of me in extreme pain. Whoa! This is good. Now to get up and get to the bathroom which was huge with a modern walk-in shower. The nurse came in before I attempted to get out of bed. I had no IV hooked up so it would be simple to disconnect from the monitor and walk to bathroom. I cannot remember this nurse’s name but she was lovely and kind. She said she would bring me some towels and I was grateful to be able to wash up. Nurse said the Physician Assistant for the Cardiac Electrophysiology would be in to see me and I would probably get released today. She was explicit that it takes time–and I was OK with that.
I received a really delicious breakfast; I guess this suite room received really good and hot meals. I was hungry but as expected could not finish because I hadn’t eaten in a while. I had also forgotten my tea bags, which I usually keep in my bag just for this hospital visits. I do not like Lipton.
I was released just after noon and actually walked out by myself. Other than having a load of black and blues on both arms, I was OK. Mike was right in front and we drove home. This was May 9th.
At home, I was tired, watched some TV and went up to bed at 7:00 pm. Scrambled or hard-boiled eggs would be my diet for at least 4 days. I didn’t have an appetite but knew I needed the protein. What happened next both surprised and depressed me. In the morning, I felt awful. Every part of my body hurt; my skin to the touch as if I had shingles. I was dizzy, nausea and weak. OK, this is day 2, I shouldn’t expect that much. I did nothing but sit in a chair, go to bed and nap, then sit in a chair again. Thinking about leaving the house was terrifying. This is not me….this is someone else recovering. I bounce back. I took some tylenol and went to bed again. So Friday and Saturday passed and I was miserable. On Saturday I walked a block; heart rate went up immediately but no afib.
I decided I would need to be patient; I had heard people recover quickly from ablations but mine was long and tedious and general anesthesia stays with you for a few days. Cocktails were not a part of life for this time and I kinda missed my gin martini.
As of today, May 17th, I am not fully recovered. The side effects of the drug I am taking are powerful. Luckily the dose has been reduced to 200 mg per day as opposed to the 800 mg I was taking for the 2 week period before the ablation. I have been told that this drug builds up in the system and remains there for a while, so I have reasoned that it is this drug making me dizzy, nauseous and weak. I have not since April 22 taken a walk longer than a few blocks. Walking now brings my heart rate up immediately and makes me uncomfortable. I went out and planted a few seeds….very slowly and deliberately. I know that my depression is caused by lack of exercise. I force myself to do something each day–I am not talking strenuous by any stretch of the imagination. So for now, no yoga, swimming, walking or Y classes. I time how much I sit and make sure that I get up and walk around the house and up and down the stairs and in the backyard. I definitely do not want to feel like this forever.
I know that the ablation takes a while to correct your heart into a sinus rhythm and I am hoping it is sooner than later. I am supported by such loving friends and family. I receive so many messages and calls each day. One day I felt so great, I sent out individual messages to many that I had a great day. I hope I can do that more often. I want to tell everyone that I am fine–but I know I am not fine every day. It will come.
Every once in a while I wonder if I did not do the TAVR procedure, what would be. It was my decision on the advise of my doctor. It was unusual that someone with severe stenosis of the aortic artery had no symptoms–I was never tired or out of breath. I was living a fine active life and I certainly hope to do that again soon.